6
The Changing Delivery of Health Care
ABSTRACT. Treatment of workplace injuries and illnesses takes place within the larger U.S. health care system, which has been undergoing dramatic changes during the past decade. One of the most striking features of health care reform has been the dramatic growth of managed care, a major element of which is tighter control on the utilization of health care services. This has led to emphases on seeing more patients (relative to preventive services, education, and research), the use of primary care physicians and other health care professionals instead of specialty-trained physicians, and the consolidation of health care into large occupational health clinics and integrated systems that provide full-time (24 hours a day, 7 days a week) coverage of workers and their families. The committee concludes that all physicians need to be more familiar with workers’ compensation and that aspiring occupational health professionals need training in managed care principles and multidisciplinary health care.
Changes in the delivery and financing of health care can have significant effects on occupational safety and health and on those who work in the field. Although some occupational safety and health workers have little contact with the health care delivery system (e.g., safety engineers), others (e.g., physicians and nurses specializing in occupational health) work in that system on a regular basis. More importantly, injured workers receive their care from health professionals and institutions that are mainstream elements of the U.S. health care system: emergency rooms, urgent-care facilities, ambulatory care and occupational health clinics, hospitals, group practices, and individual practitioners’ offices. The types of physicians involved in workers’ compensation cases can reflect the
entire spectrum available, including but not limited to all surgical specialties (orthopedists, neurosurgeons, hand surgeons, burn surgeons, etc.), emergency care physicians, family practice physicians, radiologists, physiatrists, internists, and so forth. Nurses and nurse practitioners are frequently involved in the treatment of work-related injuries, especially the minor ones. Finally, other practitioners are also involved in providing care to injured workers: chiropractors, physical therapists, occupational therapists, and acupuncturists, to name only a few. One of the continuing issues between injured workers and employers has been the control of who selects the health care providers.
Changes in the ways in which health care is delivered thus have the potential to affect not only workers’ access to care but also the cost and quality of that care. The U.S. health care system underwent dramatic changes during the decade of the 1990s. These changes were fundamental in nature and had enormous effects. They occurred rapidly and without an overall “game plan” to guide them. Three factors catalyzed the changes: the rising cost of health care, a lack of access to health care by a large and growing segment of the population, and concerns over the quality of health care.
In regard to cost, the U.S. health care system is the most expensive in the world, outstripping by more than half again the health care expenditures of any other country (Iglehart, 1999a). In 1997, U.S. health care expenditures totaled $1.092 trillion, representing 13.5 percent of the gross domestic product (GDP) (Levit et al., 1998) (Figure 6-1). Of the total, 46 percent was spent by federal, state, and local governments, with the private sector financing the rest. Premiums paid by employers and employees to purchase health insurance constituted 60 percent of the component paid by the private sector (Levit et al., 1998). In contrast to the 1980s and the early 1990s, when the annual rate of increase in U.S. health care expenditures was often in double digits, there has been a decrease in the rate of growth during the past 5 years. In 1997, for example, U.S. health care spending rose only 4.8 percent—the slowest rate of growth in more than 35 years (Iglehart, 1999a). Many are predicting, however, that this slower rate of growth will not continue. A recent study by the Health Care Financing Administration has concluded that national spending on health care will again increase at a faster rate than the rate of growth of the economy as a whole and that by 2002 it will total $2.1 trillion, or 16.6 percent of GDP (Smith et al., 1998), perhaps creating additional pressure to cut costs.
Even though the United States spends almost one-seventh of its GDP on health care, a rising number of Americans either lack health insurance or are underinsured. In 1998, 44.2 million Americans had no health insurance. This figure represented 16.3 percent of the population, an increase
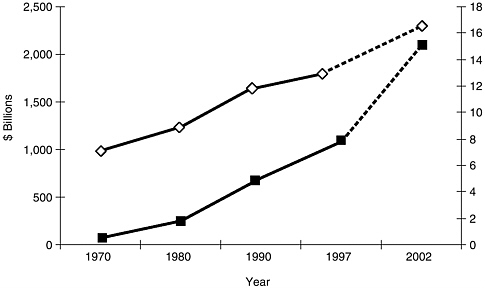
FIGURE 6-1 National expenditures for health services and supplies, 1970 to 1997 and projections for 2002, in billions of dollars (■) and as a percentage of GDP (◊).
SOURCE: Levit et al. (1998).
from 14.2 percent in 1995 (U.S. Census Bureau, 1998). Lack of insurance is closely correlated with low income (Kuttner, 1999a). Many Americans are also underinsured and must either forgo care or pay for it out of pocket. A number of recent studies have documented that the percentage of individuals who lack insurance is rising (Kuttner, 1999a).
Increases in the numbers of uninsured and underinsured individuals appear to be more closely related to a deterioration in employer-based coverage than to unemployment, since they have occurred at a time when the latter is declining (Schoen et al., 1998). Two-thirds of Americans receive their health insurance through an employer (Fronstin, 1998). The rising cost of health care has forced many employers to either drop health insurance coverage for their employees or eliminate some of the benefits that they provide. In addition, trends toward part-time or temporary employment, the growth in the number of self-employed individuals, and the contracting out of certain tasks have left many workers and their families with no or inadequate coverage. Other factors include the loss of Medicaid coverage because of welfare reform and the rising cost of “Medigap” coverage, which results in inadequate insurance coverage for elderly individuals enrolled in the Medicare program (Kuttner, 1999a).
Concerns about the quality of U.S. health care have also been a factor in promoting health care reform (Chassin et al., 1998; Bodenheimer, 1999).
Quality has been defined as “the degree to which health services for individuals and populations increase the likelihood of desired health outcomes and are consistent with current professional knowledge” (Lohr, 1990, p. 21). Poor-quality health care can occur as a result of the overuse, underuse, or misuse of health care. Although many believe that the quality of medical care for acute conditions in the United States is the best in the world, there are also substantial data to indicate that each of the factors mentioned above is still a significant problem, resulting in unnecessary morbidity and mortality (Bodenheimer, 1999). In recent years there has been a growing concern that attempts by managed care plans to reduce costs have led to underuse. There is also concern that the U.S. health care system has placed too much emphasis on the care of illness or injury after it occurs and too little emphasis on disease and injury prevention and the promotion of healthy lifestyles (Fielding, 1994).
The failure of either state governments or the federal government to enact or implement comprehensive health care reform legislation has left the private sector in control of many of the changes that are taking place in the U.S. health care system. These marketplace-initiated changes have occurred rapidly and, lacking a national consensus on what the health care system of the future should look like, have occurred in a relatively decentralized and uncoordinated fashion. They have also been controversial (Ginzberg, 1995; Angell and Kassirer, 1996; Schiff, 1996; Schroeder, 1996; Altman and Shactman, 1997; Bodenheimer and Sullivan, 1998; Blumenthal, 1999). Most observers credit them with controlling the rapid rise in health care costs but believe that they have done little to improve access to health care. There is considerable disagreement regarding their impact on the quality of health care.
ELEMENTS OF HEALTH CARE REFORM
One of the most striking features of health care reform has been the dramatic growth of managed care. There are several types of managed care organizations, including health maintenance organizations (HMOs), preferred provider organizations (PPOs), point-of-service plans (POSs), and combinations of the three. The simplest form of an HMO is a health plan that generally has its own health care clinics and providers, who are paid a salary to treat plan members. The HMO members in turn pay a fixed premium for membership and incur few if any additional costs for services received. PPOs are health plans that contract with a limited number of health care providers to provide services to plan members. Providers offer services to members on a fee-for-services basis, usually at a discount from the fees that prevail in the community. Both HMOs and PPOs typically require members to see a designated primary care provider or
other generalist before seeking the services of a specialist. POS health plans are variations of PPOs that characteristically allow a member far more freedom to choose providers, but copayments and deductibles are higher for services rendered by providers not in the plan’s network of preferred providers. Numerous other variations on these basic models exist, but common to all types of managed care organizations is tight control on the utilization of health care services. Fuchs (1997) attributes the growth of managed care organizations to two factors: rising health care costs and overcapacity in the health care delivery system. It has been estimated that 75 percent of Americans with private health insurance are enrolled in managed care plans (Iglehart, 1999a). Medicare and Medicaid have also been moving their enrollees into managed care.
Consolidation
Marketplace competition for the delivery of health care services has led to the consolidation of provider organizations. One type of consolidation, known as “vertical integration,” combines physicians and other health care professionals with hospitals, rehabilitation units, long-termcare facilities, mental health and substance abuse programs, and health promotion and disease prevention programs into an integrated whole that can deliver a comprehensive array of services. Financing mechanisms are often incorporated into these “one-stop-shopping” organizations. In addition, through mergers and buyouts there has been horizontal consolidation of health plans and integrated delivery systems into larger and larger provider entities. Through vertical integration and horizontal consolidation, provider organizations obtain marketing advantages because of a larger area and scope of coverage, have greater access to capital, and obtain economies of scale in things such as purchasing and the development of information systems. Occupational health has not escaped the consolidation movement, and recent years have witnessed an increasing concentration of occupational health and medical services in hospitals and large clinics, often part of regional or national networks.
For-Profit Health Care Organizations
Associated with consolidation in the health care industry has been the growth of for-profit health care delivery organizations (Kuttner, 1999b). Some of these investor-owned entities are newly formed, whereas others represent the conversion of not-for-profit entities to for-profit status. In 1997, 62 percent of HMO members were enrolled in investor-owned health plans (Interstudy, 1998). In the early 1990s there was rapid growth in the number of for-profit hospitals, but this trend has plateaued in re-
cent years. As of 1997, 16 percent of all U.S. hospital beds were investor owned (Kuttner, 1999b). For-profit status has been useful to the extent that it facilitates access to the capital markets, but it has been controversial because it raises the question of conflict between investors’ desire for a return on their investment and the provision of quality health care (Kuttner, 1999b).
Reimbursement
There have also been important changes in the methods of reimbursement for the provision of health care. Under the traditional U.S. health care system, providers received fee-for-service reimbursement on the basis of their charges or costs. Under the new system, payment is more likely to be through either capitation or a tightly managed fee for service at “negotiated” discount rates. Capitation places the provider at risk and discourages the provision of health care services by paying only a fixed amount per plan member regardless of the services that the member requires. An additional effect of capitation can be seen in workplaces where treatment for non-work-related injury and illness is covered through capitation and treatment for work-related injuries and illness is covered through a fee-for-service system. Under such circumstances there can be a strong incentive to classify injuries or illness as work related (Ducatman, 1986). A managed fee-for-service system also controls the provision of health services by requiring preauthorization or a second opinion before a service is delivered. A number of significant changes have also been made in Medicare and Medicaid (Iglehart, 1999b,c), including an effort to slow the previously rapid rate of growth of both programs.
Hospitals
In an effort to reduce health care costs and because of the availability of new, less invasive technologies, the site of delivery of most health care has shifted from the hospital to a variety of noninpatient settings such as clinics, physicians’ offices, outpatient surgery facilities, and the home. Occupancy rates in U.S. community hospitals fell from 64 percent in 1990 to 60 percent in 1997 (Iglehart, 1999a). Although hospital spending is still the largest single component of U.S. personal health care expenditures, it is also the slowest-growing component of an expenditure survey conducted by the Health Care Financing Administration (Iglehart, 1999a).
Specialists and Primary Care Providers
Reform of the health care delivery system has also affected the pro-
viders of health care. In the case of physicians, there has been less emphasis on specialists and specialty care and more emphasis on primary care and the role of the generalist physician (Institute of Medicine, 1996). In some cases, managed care has used generalist physicians as “gatekeepers,” without whose approval a patient cannot see a specialist. The number of other health care professionals such as nurse practitioners and physician’s assistants has increased rapidly, and their scope of practice has been expanded to include responsibilities that were previously the exclusive domain of the physician (Cooper et al., 1998a,b). This expansion of scope of practice is one example of the phenomenon of “substitution,” in which providers with less formal preparation are substituted for those with more education and training in an attempt to reduce costs. Other workforce changes include cross-training and multiskilling of health care workers and the increased use of team delivery of health care (D’Aunno, 1996).
Health Care Practices
The nature of health care has also been changing. Efforts to reduce costs and public interest in improved health have fueled a renewed emphasis on population medicine, health promotion, disease prevention, and greater integration of the various health care disciplines and public health (Rundall, 1994). There is little controversy about the relationship between lifestyle risk factors (e.g., sedentary lifestyle, tobacco use, poor nutrition, obesity, and high lipid levels) and poor outcomes that result in increased morbidity and mortality. The economic impacts of these health risks are substantial (Pelletier, 1996; Goetzel et al., 1998). Furthermore, these risk factors can be modified and workplace health promotion programs can exert a long-term positive influence on health and lifestyle practices (Heaney and Goetzel, 1997). Consequently, the growth in health promotion and disease prevention programs and counseling efforts at the work site have been both substantial and positive (Pelletier, 1996). These efforts are likely to increase as modification of risky health behaviors and cost containment are emphasized (Rogers, 1994; Kosinski, 1998).
Traditional medical practice is becoming more standardized because of evidence-based medicine, clinical practice guidelines, and disease management techniques (Ellrodt et al., 1997), but public interest in natural remedies and in alternative medicine has resulted in significant growth in the number of nontraditional health practitioners and in the widespread use of nontraditional remedies such as herbal medicines (Cooper et al., 1998a,b; Eisenberg et al., 1998; Kaptchuk and Eisenberg, 1998).
Finally, the aging of the U.S. population has increased the emphasis placed on the management of chronic disease.
Academic Health Centers
Finally, changes in the health care delivery system have had a major impact on U.S. academic health centers (AHCs). These institutions educate and train most of the nation’s health care professionals, perform large amounts of biomedical research, and provide highly specialized care in their teaching hospitals. AHCs are experiencing difficult times, in part because their traditional emphasis on the education and training of specialists and subspecialists is often out of line with the marketplace, which is emphasizing primary care and generalism. In addition, the single largest source of revenue for medical schools, the major components of most AHCs, is income derived from patient care—either through faculty practice plans or via transfers from teaching hospitals (Jones et al., 1998). It has been shown that AHC hospitals are approximately 30 percent more expensive than their nonteaching counterparts (Reuter and Gaskin, 1997). In a reformed health care system that places great emphasis on cost containment, many AHCs are having a difficult time competing for patients. To date only one AHC has been forced to close, but others are merging their programs to reduce costs and increase efficiency. If AHCs encounter severe financial difficulty in the future, their ability to maintain their programs of teaching, research, and patient care could be jeopardized. One result could be impairment of their programs in occupational safety and health education, training, and research.
Managed Care in Workers’ Compensation
Nationwide, the costs of workers’ compensation doubled between 1985 and 1990 (Soloman, 1993), and beginning in 1991 states began to pass legislation that allowed or required workers’ compensation programs to copy the cost-control techniques of managed care group health plans. The earliest efforts at cost control involved the implementation of discounted fee schedules for providers and health facilities. A 1996 study by the Workers Compensation Research Institute (Burton, 1996) found that fee schedules had been introduced in 40 states and that hospital billing regulations had been introduced in 35 states. From the little research available, it appears that fee schedules have not reliably reduced medical costs, as providers in the predominantly fee-for-service systems delivered more or more complex services per case, offsetting the lower fees for each service imposed by the schedule (Nikolaj and Boon, 1998).
Subsequent approaches to managing health care in workers’ compensation cases have turned to networks of preferred providers, treatment guidelines, aggressive case management, and 24-hour coverage (Dembe, et al., 1998; Leone and O’Hara, 1998; Nikolaj and Boon, 1998; Weinper,
1999). Nikolaj and Boon (1998) report that 48 states now limit workers’ choice of providers in some way (the employer or the insurer chooses the provider or restricts the employee’s initial selection or freedom to change providers). There are as yet no definitive answers to the questions of whether limiting choice decreases costs or has any effect on the quality of care (limiting choice to occupational medicine specialists would presumably increase the quality of care and reduce costs through prevention programs and more aggressive rehabilitation). Standardization of treatment through data-driven guidelines is another cost-control technique with the potential to improve treatment as well, given that most patients who are free to choose a provider are likely to be treated by a primary care provider with little or no training in occupational health and safety principles (Hashimoto, 1996). Case management, that is, the systematic coordination of medical, rehabilitative, and social services, assumes added importance in workers’ compensation cases, in which medically unnecessary delays in return to work mean costly disability payments for the insurer and decreased income for most patients (Christian, in press). Note that under these circumstances, a narrow focus on cutting medical costs by reducing services may in fact increase overall costs by delaying return to work. Eccleston (1995) reports that case management is required in about half the states that regulate managed care. Yet another experiment at cost control has been 24-hour coverage—integration of workers’ compensation and group health coverage by using the same resources for both personal and work-related health care. In theory, this approach has a number of advantages, including cost savings from consolidation of administration, elimination of “double-dipping,” reduction in cost shifting, and consistency and continuity of care. In practice, fundamental differences in the two systems (for example, the high cost of disability compensation that can outweigh savings from less than aggressive medical treatment) have limited adoption of this sort of consolidation (Leone and O’Hara, 1998).
Several studies made systematic attempts to assess cost savings subsequent to changes in the manner in which health care was provided. In all cases, however, numerous changes were introduced simultaneously, which makes it impossible to judge their relative contributions to subsequent cost savings and other effects. A well-documented pilot project in the state of Washington changed the method of payment from fee for service to capitation and required workers to use the occupational medicine clinics of one of two large managed care organizations (Sparks and Feldstein, 1997). A similar study in Maryland (Green-McKenzie et al., 1998) looked at two cohorts of injured workers before and after the introduction of a managed care initiative involving an on-site case management team, a preferred provider network, and safety engineering and
ergonomics programs. Both of these experiments showed large decreases in employer or insurer expenditures, both medical payments and disability payments. Quality of care was not directly assessed in either study, but the Washington study included telephone interviews with injured workers at 6 weeks and 6 months after injury. No significant differences between the intervention and control groups were seen in reports of pain, mental health, or physical functioning at either time, but at 6 weeks the workers receiving treatment through the managed care organizations were somewhat less satisfied with their treatment overall and their access to care. The Maryland study reports only that despite freedom to opt out at any time, 99 percent of the injured workers in the managed care group chose to stay within the system. Also of note is the fact that the number of claims was actually higher in the managed care cohort, so it is unlikely that the large cost savings were simply the result of a denial of claims.
Twenty-nine states currently have some type of managed care program for workers’ compensation, costs to insurers and employers are down (Mont et al., 1999), and workers’ compensation is once more a profitable sector for insurers (National Council on Compensation Insurance, as cited by Consumer Reports, 2000). Managed care is thus very likely to be a major part of workers’ compensation for the foreseeable future.
IMPLICATIONS FOR EDUCATION AND TRAINING OF OCCUPATIONAL SAFETY AND HEALTH PROFESSIONALS
It is difficult to say with confidence that the market-driven changes in health care delivery will continue to evolve with cost reduction as its major theme. Signs of competition on the basis of quality, as well as increasing pressure on governments to intervene with “patient bills of rights” and more specific mandates like those that prohibit “drive-through” births, suggest that the pendulum may have started to swing away from cost cutting as a prime mover. Nevertheless, there are a number of features of U.S. health care today that are likely to affect the occupational safety and health workforce, primarily that segment dealing with the clinical care of workers, for some time to come.
First, the promise of population-based medicine and a corresponding emphasis on prevention certainly imply a favorable climate for occupational safety and health, but in practice this promise has, by and large, not been fulfilled. High rates of turnover of health plan members have undermined the assumed long-term savings achieved from the use of preventive measures like vaccinations, since the recipient will likely belong to a rival plan when the benefits are realized.
Second, the need to generate revenue and save money has led to an emphasis on seeing more patients—a trend reflected in the data in Chap-
ter 2, which indicate that occupational medicine physicians are increasingly employed by clinics and less often by industry. The Association of American Medical Schools has frequently expressed the view that this increased emphasis on seeing patients is interfering with the conduct of the research and education missions at academic health centers. It may compete with the preventive aspects of occupational health as well.
Third, emphasis on primary care physicians, nurse practitioners, physician’s assistants, and other health care professionals instead of specialist physicians may undermine attempts to increase the small numbers of board-certified occupational medicine specialists. As an earlier Institute of Medicine report (Institute of Medicine, 1988) pointed out, increasing the ability of primary care physicians in occupational medicine is vital for the health and safety of workers, but that task is itself dependent on a larger supply of occupational medicine specialists. A similar argument applies to the undeniable need for more coverage of occupational safety and health in physician’s assistant and nurse practitioner training.
Fourth, the use of teams to deliver health care means that occupational safety and health training programs should expose students to the delivery of health care by teams.
Fifth, the growth of managed care means that more occupational safety and health services (including those paid for by workers’ compensation) will be delivered in a managed care setting, so occupational safety and health students should be exposed to managed care during their training programs. Rivo et al. (1995) and Meyer et al. (1997) propose new curricula that can be used to better prepare physicians for practice in the managed care setting.
Sixth, occupational safety and health students should understand health care financing and the pressure to reduce health care costs and the likely impact of these on the quality of occupational health services.











